Obstructive Sleep Apnea: Causes, Treatments & Health Risks
Published:
Obstructive sleep apnea (OSA) is a prevalent and potentially severe slumbering disorder that manifests itself in repeated occurrences of partial or full upper airway obstruction during rest, causing disjointed breathing. This condition affects millions of people worldwide, causing excessive daytime sleepiness, reduced quality of life, and increased risk for cardiovascular diseases. In this comprehensive blog post, we will delve into the causes and severity levels of OSA while shedding light on its prevalence among different demographics.
Contents:
- Understanding Obstructive Sleep Apnea
- Causes of obstructive sleep apnea
- The Prevalence of Obstructive Sleep Apnea
- The Prevalence of Obstructive Sleep Apnea
- Treatment Options for Obstructive Sleep Apnea
- Continuous Positive Airway Pressure (CPAP) Therapy
- Weight Loss Interventions For Diabetic Patients With OSA
- The Impact of Obstructive Sleep Apnea on Cardiovascular Health
- FAQs in Relation to Obstructive Sleep Apnea
- Obstructive Sleep Apnea (OSA)
- OSA Risk Factors
- Health Risks Associated with OSA
- OSA Diagnosis
- OSA Treatment Options
We will also explore various treatment options available for individuals suffering from OSA, including behavioral measures for mild cases as well as advanced therapies such as continuous positive airway pressure (CPAP) devices. Furthermore, we will discuss the importance of weight loss interventions in managing obstructive sleep apnea among diabetic patients and highlight the impact that untreated OSA can have on one's cardiovascular health.

Understanding Obstructive Sleep Apnea
Owing to its diverse and inconspicuous manifestations, OSA is a widespread disorder that can have severe metabolic and cardiovascular repercussions. It occurs when the muscles in the throat relax, causing partial or complete blockage of airflow during sleep. Millions of individuals suffer from OSA, yet it is often not detected due to the mild signs such as fatigue in the day, morning migraines and snoring.
Causes of obstructive sleep apnea
The primary cause of OSA is a relaxation of the muscles in the upper airway during sleep, leading to an obstruction that prevents normal breathing. Several factors contribute to this muscle relaxation, including obesity, alcohol consumption before bedtime, smoking, family history of OSA or other sleep disorders, nasal congestion or anatomical abnormalities like enlarged tonsils.
Mild vs severe obstructive sleep apnea
- Mild OSA: Individuals with mild obstructive sleep apnea experience five to 14 episodes per hour where their breathing stops for at least ten seconds each time. Symptoms may include occasional snoring and disrupted nighttime rest but are generally less noticeable than those experienced by individuals with more severe cases.
- Severe OSA: Severe cases involve frequent pauses in breathinga€”30 times per hour or morea€”and result in significant oxygen deprivation throughout the night. This level poses serious health risks such as heart disease, stroke,heart failure,,and cardiovascular disease. Severe OSA patients may also experience extreme daytime sleepiness, making it difficult to function during the day.
A diagnosis of OSA may be made through a home sleep apnea test or an overnight stay at a sleep center, where doctors can track breathing and other physiological factors during rest.
The Prevalence of Obstructive Sleep Apnea
As obesity rates rise globally, so does the prevalence of OSA. In Europe, one study found that approximately 1,152,539 individuals were treated for OSA using CPAP therapy in just one year alone - indicating its widespread impact on healthcare systems (source). Obesity is a significant contributing factor due to excess fatty tissue around the neck and throat area leading to airway obstruction.
Gender differences in prevalence
Males: Men are more likely than women to develop obstructive sleep apnea due to hormonal differences and anatomical factors such as larger neck circumference and narrower airways.
Females: Women tend to have lower rates of OSA overall but are at higher risk after menopause when hormone levels change significantly.
The Prevalence of Obstructive Sleep Apnea
As obesity rates rise globally, so does the prevalence of obstructive sleep apnea (OSA). In Europe, one study found that approximately 1,152,539 individuals were treated for OSA using CPAP therapy in just one year alone - indicating its widespread impact on healthcare systems. Understanding the contributing factors and differences in prevalence among various populations is essential to address this growing health concern.
Obesity as a Contributing Factor
Obesity, particularly central obesity characterized by excess abdominal fat, has been identified as a major risk factor for developing obstructive sleep apnea. The accumulation of fatty tissue around the neck can cause narrowing or obstruction of the upper airway during sleep. According to research published in Sleep Medicine Reviews, an estimated 60-90% of adults with OSA are obese.
- A greater BMI can heighten the risk of and aggravate OSA.
- Losing weight can significantly improve or even eliminate symptoms associated with sleep-disordered breathing.
- Keeping active and eating a balanced diet are essential for avoiding illnesses like OSA that can be linked to obesity.
Gender Differences in Prevalence
In addition to obesity, gender plays a significant role in determining susceptibility to obstructive sleep apnea. Males are more prone to OSA than females, with the prevalence estimated at two to three times higher. This disparity can be attributed to several factors:
- Men tend to have a larger neck circumference and more fat deposition around the upper airway, increasing their risk of developing sleep apnea.
- Hormonal differences between men and women may also contribute to variations in OSA prevalence. For example, estrogen is believed to protect against airway collapse during sleep.
- Postmenopausal women, due to age-related hormonal changes, are at an increased risk of developing OSA compared to premenopausal women.
In conclusion, it is essential for healthcare providers and individuals alike to recognize the growing prevalence of obstructive sleep apnea as a serious public health concern. By understanding contributing factors such as obesity and gender differences, targeted interventions can be developed for those at highest risk - ultimately reducing associated health complications like excessive daytime sleepiness, heart failure, and cardiovascular diseases in patients suffering from this common disorder.

Treatment Options for Obstructive Sleep Apnea
Depending on the severity and individual needs, treatment options range from lifestyle changes like weight loss and exercise to medical interventions such as positive airway pressure devices or surgical procedures. Early diagnosis and appropriate management are crucial for reducing health risks associated with untreated OSA.
Behavioral Measures for Mild Cases
In mild cases of OSA, simple behavioral measures may be sufficient in alleviating symptoms and improving overall sleep quality. Some effective strategies include:
- Maintaining a healthy body weight through diet and exercise
- Avoiding alcohol consumption close to bedtime, as it relaxes throat muscles
- Sleeping on one's side instead of the back to prevent airway obstruction
- Practicing good sleep hygiene by establishing regular sleeping patterns and creating a comfortable sleep environment.
Positive Airway Pressure Devices (PAP)
Continuous Positive Airway Pressure (CPAP) therapy is considered the gold standard treatment option for moderate-to-severe OSA patients. These machines work by delivering continuous airflow through a mask worn over the nose or mouth during sleep, keeping the upper airways open and preventing episodes of interrupted breathing.
Besides CPAP therapy, other types of PAP devices are available depending on patient preferences or specific needs:
- Bilevel Positive Airway Pressure (BiPAP): This PAP device offers two distinct pressure levels - higher when inhaling and lower while exhaling, making it more comfortable for certain patients.
- Adaptive Servo-Ventilation (ASV): An advanced PAP device that continuously adjusts pressure levels based on the patient's breathing patterns, suitable for those with central sleep apnea or complex sleep apnea syndrome.
Oral Appliances Holding Jaw Forward During Sleep
Mandibular advancement devices (MADs) are custom-made oral appliances designed to hold the lower jaw forward during sleep. This helps keep the airway open by preventing the tongue from falling back into the throat. MADs can be an effective alternative treatment option for mild-to-moderate OSA cases in patients who cannot tolerate CPAP therapy or prefer a less invasive approach.
Surgical Modification Options
In certain situations, surgical interventions may be necessary to treat OSA effectively. Some common procedures include:
- Uvulopalatopharyngoplasty (UPPP): A procedure that removes excess tissue from the soft palate and uvula to enlarge the upper airway.
- Tonsillectomy and/or adenoidectomy: The removal of tonsils and/or adenoids if they contribute to airway obstruction during sleep.
- Genioglossus Advancement (GA): A surgery that repositions part of the tongue muscle attachment forward, increasing space at the back of throat and reducing chances of obstruction during sleep.

Continuous Positive Airway Pressure (CPAP) Therapy
One of the most effective treatments for obstructive sleep apnea is Continuous Positive Airway Pressure (CPAP) therapy. This method involves using a machine that delivers continuous airflow through a mask worn over the nose or mouth during sleep, ensuring an open airway and preventing breathing interruptions. CPAP has been proven to not only improve quality of life but also reduce long-term health complications associated with chronic untreated sleep apnea.
How CPAP Works for Treating Sleep Apnea
The primary function of CPAP machines is to provide positive air pressure into the upper airways, preventing them from collapsing during sleep. The apparatus includes a motor for creating pressurized air, connecting tubing linking the engine to the mask, and an ergonomic face-covering designed to fit securely on your nose or mouth. When you breathe in while wearing this apparatus, it provides enough pressure to keep your throat muscles from relaxing too much and blocking airflow.
Benefits & Effectiveness
- Better Sleep Quality: By maintaining an open airway throughout the night, CPAP users often experience fewer awakenings due to breathing disruptions and report improved overall sleep quality.
- Increase Daytime Alertness: With more restful nights comes increased daytime alertness as well as reduced excessive daytime sleepiness - both common symptoms experienced by those suffering from untreated sleep apnea.
- Lowers Blood Pressure: Studies have shown that consistent use of CPAP can help lower blood pressure levels in individuals with hypertension related to their sleep apnea condition (source).
- Reduced Cardiovascular Risks: As mentioned earlier, untreated sleep apnea can lead to various cardiovascular diseases. CPAP therapy has been shown to reduce the risk of heart failure and other complications by effectively managing sleep-disordered breathing.
- Morning Headache Relief: Many people with sleep apnea often experience morning headaches due to low oxygen levels during sleep. Regular use of a CPAP machine can help alleviate this symptom as it ensures adequate airflow throughout the night.
For maximum effectiveness, CPAP users should collaborate with their healthcare providers to ensure proper use of the device and any supplemental therapies. This includes regular cleaning and maintenance of equipment, adjusting pressure settings if needed, and ensuring a comfortable fit for optimal adherence. Additionally, some individuals may benefit from supplemental therapies such as lifestyle changes or oral appliances in conjunction with their CPAP treatment plan (source). By taking these steps towards effective management of sleep apnea through continuous positive airway pressure devices like nasal CPAP machines or full face masks options, patients can significantly improve both their quality of life and overall health outcomes.
Weight Loss Interventions For Diabetic Patients With OSA
Diabetic patients are often affected by OSA, and weight loss interventions can be an effective means of managing it. One of the most effective ways to manage OSA in these individuals is through weight loss interventions. This article will discuss the value of shedding pounds in treating OSA and give tips for successful weight control.
Importance of Weight Loss in Treating OSA
Studies have shown that obesity is a major risk factor for developing obstructive sleep apnea, as excess body fat can cause airway obstruction during sleep. Losing weight not only helps alleviate symptoms associated with OSA but also improves cardiovascular health and reduces the risk of other complications related to diabetes.
- Losing just 10% of body weight can lead to significant improvements in both daytime sleepiness and nighttime breathing disturbances caused by obstructive sleep apnea.
- A study published in the journal Sleep Medicine Reviews found that losing at least 15% of initial bodyweight led to an improvement or even complete resolution of mild-to-moderate cases of obstructive sleep apnea.
- In addition to improving respiratory function during sleep, achieving a healthy BMI has been linked with better glycemic control - essential for managing diabetes effectively.

Strategies for Successful Weight Management
To achieve lasting results when it comes to shedding excess pounds, adopting sustainable lifestyle changes is key. Here are some evidence-based strategies that diabetic patients with obstructive sleep apnea should consider:
- Dietary modifications: Consuming a balanced diet rich in whole grains, lean proteins, fruits, and vegetables is crucial for weight loss. Diabetic patients should also pay close attention to portion sizes and carbohydrate intake to maintain optimal blood sugar levels.
- Physical activity: Engaging in regular exercise not only aids weight loss but can also help improve sleep quality. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week for adults.
- Sleep hygiene: Establishing a consistent sleep schedule and creating an environment conducive to restful sleep can help alleviate symptoms associated with obstructive sleep apnea. This includes avoiding caffeine and alcohol before bedtime, keeping the bedroom cool and dark, and removing electronic devices from the sleeping area.
- Bariatric surgery: In cases where lifestyle changes alone are insufficient for achieving significant weight loss, bariatric surgery may be considered as an option. After assessing your BMI, OSA severity and comorbidities like heart disease or hypertension, it may be necessary to consider bariatric surgery as an option.
Incorporating these strategies into daily life can greatly benefit diabetic patients suffering from obstructive sleep apnea by promoting sustainable weight loss that leads to improved health outcomes overall.
The Impact of Obstructive Sleep Apnea on Cardiovascular Health
Untreated or inadequately managed obstructive sleep apnea (OSA) can lead to hypertension, stroke, heart failure, and other cardiovascular complications. Early diagnosis and appropriate treatment are essential for reducing these risks while improving the overall quality of life for affected individuals.
The Connection Between Hypertension and Obstructive Sleep Apnea
Research has shown that there is a strong link between OSA and the development of hypertension. When breathing stops during an episode of sleep apnea, oxygen levels in the blood drop significantly. This triggers a stress response in the body that leads to increased production of adrenaline and cortisol - hormones known to raise blood pressure. Additionally, repeated episodes of low oxygen levels cause inflammation within blood vessels which further contributes to elevated blood pressure.
- Prevalence: Studies have found that up to 50% of people with OSA also suffer from hypertension.
- Risk Factors: Obesity is a major risk factor for both conditions; however, factors such as age, gender, family history, and lifestyle habits also play a role in their development.
- Treatment Benefits: Effective management of OSA through continuous positive airway pressure (CPAP) therapy or other treatments can help lower high blood pressure in many cases.
Reducing Cardiovascular Risk Through Proper Management
In addition to hypertension, untreated OSA has been linked with various cardiovascular diseases including coronary artery disease (CAD), heart failure, and stroke. The repeated episodes of low oxygen levels during sleep can cause damage to the lining of blood vessels, leading to plaque buildup in the arteries (atherosclerosis) and increasing the risk for CAD.
Furthermore, untreated OSA has been associated with an increased risk of developing atrial fibrillation, a type of irregular heartbeat that can lead to heart failure or stroke if left unmanaged. Atrial fibrillation occurs when there is disorganized electrical activity within the upper chambers (atria) of the heart, causing them to quiver instead of contracting effectively.
To reduce cardiovascular risks associated with obstructive sleep apnea:
- Seek early diagnosis: If you suspect you may have OSA due to symptoms such as loud snoring, gasping for air during sleep, or excessive daytime sleepiness, consult your healthcare provider for a proper evaluation.
- Adhere to treatment plans: Follow your doctor's recommendations regarding CPAP therapy or other treatments prescribed for managing your condition.
- Maintain a healthy lifestyle: Adopting habits such as regular exercise, maintaining a balanced diet, and avoiding tobacco use can help improve both OSA severity and overall cardiovascular health.
FAQs in Relation to Obstructive Sleep Apnea
What is obstructive sleep apnea commonly associated with?
Other factors include age, family history, alcohol consumption, smoking, and certain medical conditions like hypothyroidism or acromegaly. To learn more about OSA risk factors, click here.
What is an obstructive sleep apnea journal?
An obstructive sleep apnea journal refers to a scientific publication that focuses on research related to OSA. These journals publish studies exploring causes, symptoms, treatments, and prevention strategies for this condition. Examples of such publications include the Journal of Clinical Sleep Medicine and Sleep & Breathing. To learn more about OSA, click here.
What is the life expectancy of someone with sleep apnea?
The life expectancy of someone with untreated sleep apnea may be reduced due to increased risks for cardiovascular disease, stroke, and other health complications. However, early diagnosis and proper treatment can significantly improve quality of life and reduce these risks. It's essential to consult a healthcare professional if you suspect you have OSA. To learn more about the health risks associated with OSA, click here.
Can you reverse obstructive sleep apnea?
In some cases, yes - lifestyle changes like weight loss through diet modification or exercise can help reverse mild-to-moderate OSA by reducing airway obstruction caused by excess fat tissue in the throat area (source). In severe cases, medical interventions like CPAP therapy or oral appliances may be necessary to manage the condition effectively. To learn more about OSA treatment options, click here.
Obstructive Sleep Apnea (OSA)
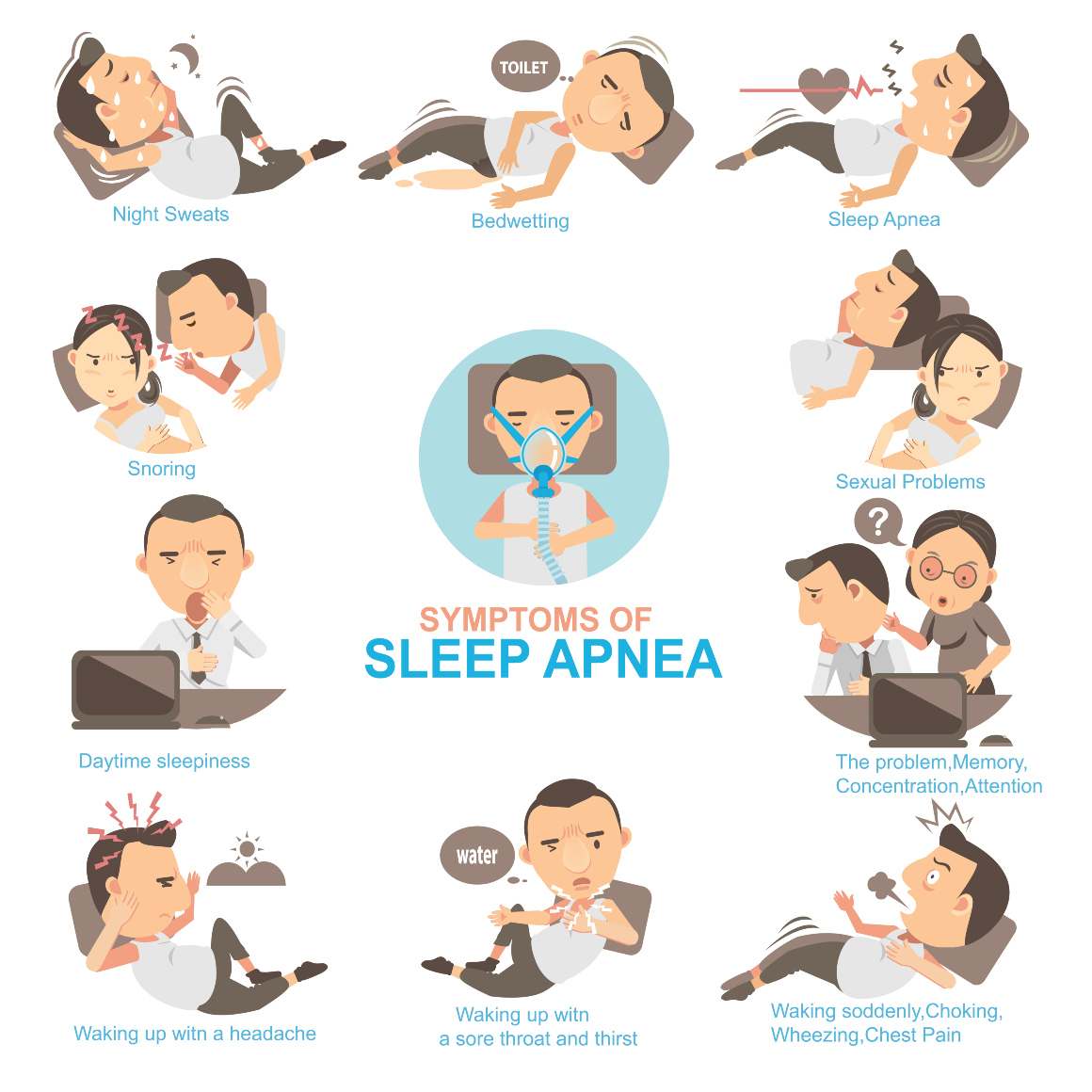
This can lead to a range of symptoms, including:
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating
- Memory problems
- Depression
OSA is diagnosed through a sleep study, which can be done in a sleep center or through home sleep apnea testing. To learn more about OSA diagnosis, click here.
OSA Risk Factors
OSA is associated with a range of risk factors, including:
- Obesity
- Age
- Family history
- Alcohol consumption
- Smoking
- Certain medical conditions like hypothyroidism or acromegaly
It's important to be aware of these risk factors and to consult a healthcare professional if you suspect you have OSA. To learn more about OSA, click here.
Health Risks Associated with OSA
Untreated OSA can lead to a range of health complications, including:
- Cardiovascular disease
- Stroke
- Heart failure
- High blood pressure
- Type 2 diabetes
Early diagnosis and proper treatment can significantly reduce these risks. To learn more about OSA treatment options, click here.
OSA Diagnosis
OSA is diagnosed through a sleep study, which can be done in a sleep center or through home sleep apnea testing. During a sleep study, various parameters are measured, including:
- Apnea-hypopnea index (AHI)
- Oxygen saturation levels
- Heart rate
- Respiratory effort
Based on the results of the sleep study, a healthcare professional can determine the severity of OSA and recommend appropriate treatment options. To learn more about OSA treatment options, click here.
OSA Treatment Options
OSA treatment options include:
- Lifestyle changes (e.g., weight loss, exercise)
- Positive airway pressure (PAP) therapy (e.g., nasal CPAP)
- Oral appliances
- Surgery
The most appropriate treatment option depends on the severity of OSA and other individual factors.








